Post Bariatric Surgery Diet & Nutrition | Clinic Antalya

Here, you will find:
Gastric Bypass & Sleeve Gastrectomy
- The Surgeries ................................................................
- Skills for Success............................................................
- Physical Activity...............................................................
Post op Diet Stages
- Stage 1: Fluids ..............................................................
- Stage 2: Protein Shakes ...............................................
- Stage 3: Soft Textures ..................................................
- Vitamin/Mineral Supplements........................................
- Stage 4: Regular Textures .............................................
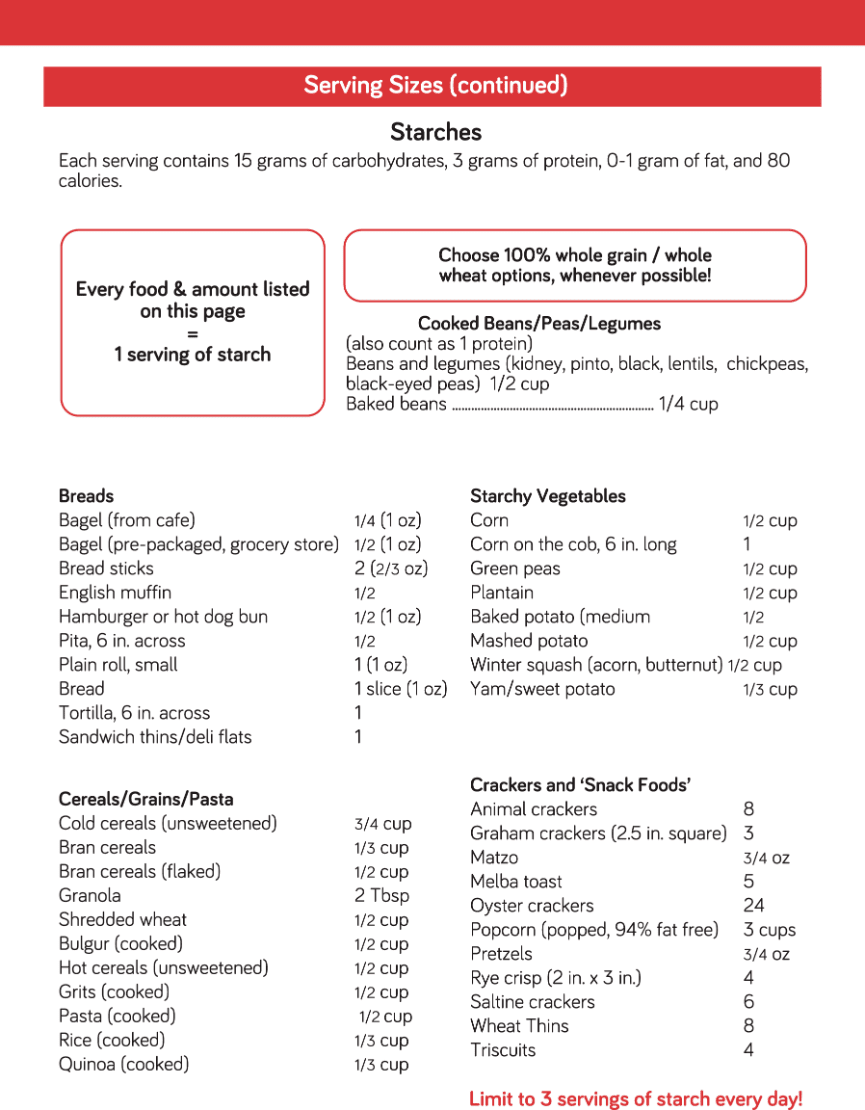
- Serving Sizes ................................................................
- Possible Problems and Solutions ..................................
Offered Dietitian Appointment Schedule*
Before Surgery:
- Nutrition Assessment
After Surgery
- 1 st month
- 3 th month
- 6 th month
- 9 th month
- 1 year
- After 1 year, twice per year (every 6 months) for lifetime
The Surgeries
There are two main surgical options which help you to lose weight and become healthier. They are gastric bypass and sleeve gastrectomy.
- Restriction – Your smaller stomach will limit food you can eat in one sitting. The restriction will decrease over years, so you will need to rely on healthy lifestyle habits.
- Metabolic Changes – Stomach hormones and some other signals in your body change after surgery. This can make people feel less hungry and helps health conditions like diabetes. Your body can adapt to this change in gut hormones and you will probably feel hunger again over time.
Hospitalization period is 2-4 nights after gastric bypass or sleeve gastrectomy.
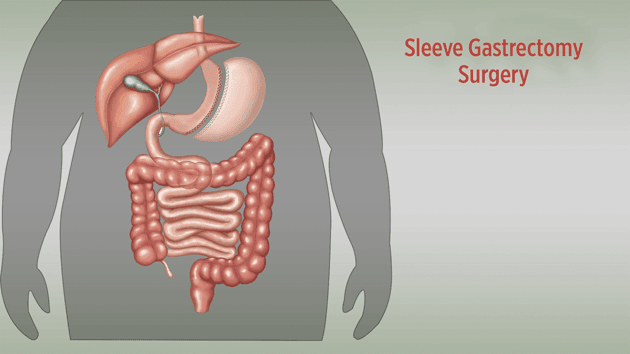
Sleeve gastrectomy is based on the reduction of stomach volume.
This restrictive method is more physiological than others.
Lowering the level of Ghrelin hormone provides the feeling of satiety.

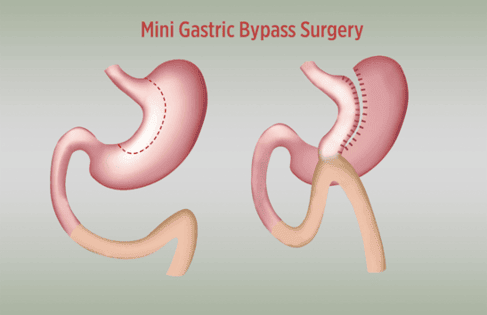
The aim of a gastric bypass operation is to reduce the amount of food intake by reducing the stomach volume and connecting the small intestine to the small stomach pouch, this aims to shorten the path of food that is absorbed.
Skills for Success
Bariatric surgery is your supporter. You must commit to a healthy lifestyle (proper eating habits, exercise, behaviors) to stay successful forever.
Fluids
- Choose sugar-free, non-carbonated fluids.
- Sip fluids throughout the day.
- Know the signs of dehydration: Headaches, dizziness, dark urine.
- No caffeine until stage 4.
- Avoid alcohol after surgery.
Eating Behaviors
- Take bites the size of a dime.
- Chew your food thoroughly, puree the food with your teeth.
- Wait between bites to see how your stomach feels.
- Aim for 30-40 minute meals.
Make Eating Mindful
- Avoid grazing, nibbling, and picking throughout the day.
- Have regularly scheduled eating events.
- When you’re eating, just eat! Avoid distractions.
Separate Fluids From Solids
- Wait to drink fluids until 30 minutes after you eat solid food.
- It’s okay to drink before eating.
- Why? Eating and drinking at the same time can overfill your stomach and make you feel sick.
Plan Ahead
- Life is busy now and it will be busy after surgery too.
- Make healthier choices.
- Pack food and fluids for busy days.
Physical Activity
Most people need to exercise at least 4 hours each week to maintain weight loss. You can even break your exercise up into smaller amounts of time during the day. It's about finding what works best for you.
Here are some ideas for increasing your physical activity before and after surgery.*
- Walk more!
- Wear a pedometer to track your steps and challenge yourself to increase steps over time.
- Take a "walking break" at work instead of a coffee break.
- If you take the bus or subway, get off a few stops early and walk.
- Park your car farther away at shopping centers and walk through the parking lot.
- Take the stairs instead of the elevators.
- Make exercise a family event. Go for a walk together after dinner or on the weekend.
- To decrease impact on your joints, try pool exercises, water aerobics, or a stationary bicycle.*
- Check out exercise videos online.
What are the benefits of exercise besides weight control?
- Improves mood • Keeps body strong • Improves bone health
- Boosts energy • Promotes better sleep • Improves heart health
* Remember to check with your primary care doctor or surgeon before starting any strenuous exercise. However, you may start walking right after surgery. Also you may swim and all other exercises 4 weeks after surgery.
Post-Op Diet Stages
Stage 1 : Fluids - Starts in hospital
Stage 2 : Protein Shakes and soup - Starts in hospital
Stage 3 : Soft Textures - Starts 14 days after surgery
Stage 4 : Regular Textures - Starts at 5 th week after surgery
Post-Op Diet Stage 1 : Fluids
Starts: In the hospital on the first day after surgery.
What to do: Sip sugar-free, non-carbonated, non-caffeinated fluids throughout the day.
Example of fluids
- Broth (If it comes heavy, a few drops of lemon can be squeezed).
- Chicken broth (If it comes heavy, a few drops of lemon can be squeezed).
- Skim milk (lactose free).
- Without grains, without pulp, low calorie soups with water consistency.
- Foamless, non-carbonated less sugary / sugar free fruit drinks.
- Unsweetened pure fruit juices (freshly squeezed, without froth, apple juice)
- Sugar free tea (warm)
- Hulless grains
- Herbal teas (warm)
- Vegetable juice (consume dilute)
You should consume warm drinks !!
You will be in the hospital for this entire diet stage and you will be given the right types of fluids. The nurses will guide you to sip enough fluids during the day.
Stage 1 Key Points:
- Fluids are the number one priority!!
- You will only be able to sip small amounts of fluid at one time.
Pace yourself throughout the day.
- Gulping and chugging fluids will cause stomach pain.
- Avoid caffeine until Stage 4. It irritates the stomach.
- Carbonation can cause gas, belching, bloating, and stomach discomfort.
Some people never tolerate carbonation after surgery.
- You can use artificial sweeteners such as Equal, Sweet & Low, Splenda, PureVia and Truvia (Stevia), and Nectresse (monk fruit).
Post-Op Diet Stage 2: Protein Shakes and Soup
Starts: In the hospital on the third day after surgery.
Lasts for: 14 days
What to do: Sip fluids throughout the day. Eat soup and broth 3-4 times. Drink a protein shake 2 times per day. If you haven’t finished the protein shake after one hour, stop drinking it. Fluids are still the number one priority.
Fluid Goal: 48-64 ounces(1500ml) (fluid guidelines listed in stage 1). This does not include your protein shakes.
Protein Goal: 60-70 grams (number of shakes per day depends on the brand of the protein shake)
It is normal to not reach your fluid and protein goals right away. Just do your best each day.
Protein Shake Nutrition Guidelines Each protein shake* should have:
- At least 15 grams of protein
- 100-200 calories
- Less than 20 grams of sugar
* A typical protein shake is 8-11 ounces (235-325 ml).
Post-Op Diet Stage 2: Protein Shakes (continued)
Lactose Intolerance:
Lactose is the natural sugar in milk. Sometimes after surgery, your body cannot digest this sugar. This causes problems like nausea, cramping, bloating, gas, and/or diarrhea. It is not normal to have these problems from drinking protein shakes. You might be experiencing lactose intolerance.
What if you are experiencing lactose intolerance?
- Stop drinking protein shakes for 24 hours. Keep drinking your fluids.
- When you start drinking protein shakes again, avoid any shakes that have milk, whey protein concentrate or milk protein concentrate in the ingredient list.
- Instead, choose a protein shake that is made from whey protein isolate. The lactose has been filtered out of whey protein isolate.
- Call your dietitian if you need help finding lactose-free options.
Having Trouble with Protein Shakes?
If the taste is bothering you:
- Flavor your shakes with extracts. You can find extracts in the baking aisle at the grocery store. You only need a couple of drops, so go slowly and taste-test along the way.
- Flavor your shakes with sugar-free syrups. You can find sugar-free syrups at the grocery store but you will have more flavor options if you order online.
- Flavor your shakes with spices, such as cinnamon, ginger, nutmeg, and cloves.
- Flavor your shakes with unsweetened cocoa powder or powdered peanut butter; limit to 1 tablespoon total per day.
If the smell is bothering you:
- Drink your shake from a bottle with a small opening.
- Drink your shake using a milkshake flask.
- Drink your shake at a very cold temperature.
If you need to chew:
- Pour your protein shake into a popsicle or ice cube tray and freeze to make a protein popsicle.
- Semi-freeze your protein shake or blend it with ice to make a slushy.
Stage 2 Key Points:
- Be aware of signs of dehydration: sudden lightheadedness or dizziness, headaches, and urine color becoming darker throughout the day.
- If you’re struggling to tolerate fluids, it’s helpful to try different temperatures for your beverages. Some patients prefer ice cold while others prefer room temperature or warmer beverages.
- Keep track of the amount of protein shakes and fluids that you are drinking, using a food log. If you cannot finish a protein shake in a one hour period, you can save it for the next meal time.
- Changes in bowel regimens, such as less frequent movements or loose stools, are normal. If you are having discomfort, contact the bariatric team.
Example menu
08:00 1 CUP MILK (OIL OR LACTOSE FREE) + PROTEIN POWDER
10:00 1 CUP FRESH FRUIT JUICE OR VEGETABLE JUICE
12:00 1 CUP MEAT / CHICKEN JUICE (LEMON CAN BE DRIZZLED)
14:00 1 CUP AYRAN (FLOURED YOGHURT)
16:00 1 CUP MILK (OIL OR LACTOSE FREE) + PROTEIN POWDER
18:00 1 CUP MEAT / CHICKEN WATER SOUP (LEMON DRIZZLE)
20:00 1 CUP MILK (OIL OR LACTOSE FREE) + PROTEIN POWDER
22:00 1 CUP FRESH FRUIT JUICE OR VEGETABLE JUICE
Post-Op Diet Stage 3: Soft Textures
Starts : 14 days after your surgery date
Lasts for : 30-35 days
What to do : Keep sipping fluids. Have a protein shake or eat a protein food 4-5 times per day. Start taking vitamin and mineral supplements. Please only eat the foods listed on this page.
Fluid Goal : 48-64 ounces(1300ml-1700ml) (fluid guidelines listed in stage 1)
Protein Goal : 60-70 grams/day
Third Week Foods you can consume (In addition to the first and second weeks) !!!
* Prepared without flour and tomato paste, using blender. Ex: Fish soup, lentil soup, chicken broth soup, vegetable soup, yogurt without rice soup etc…
Protein Foods
- Fat-free yogurt (without fruit chunks)
- Low-fat cottage cheese
- Part-skim ricotta cheese
- Tofu
- Vegetarian refried beans (black or pinto)
- Protein shakes and powders
- Chicken or turkey
- Fish (Tuna, salmon)
- Egg whites or egg beaters
Non-Protein Foods
- Fat-free or light yogurt. Try to meet the protein goal of 60-70 grams / day.
- Unsweetened applesauce.
- Canned pears or peaches (in own juice or water; no syrup) foods from this list.
- Soft banana will fill up quickly from the protein.
- Oatmeal, cream of wheat, or farina foods.
- Sugar-free puddings.
Stage 3 Key Points :
- Remember to drink plenty of fluids to stay hydrated and wait to drink fluids until 30 minutes after food.
- You might not feel hungry, but you still need to eat regularly.
- Space out your eating events evenly during the day.
- Some days you won’t have room for everything. Do your best to reach your protein goal.
- Stop eating or drinking at the first sign of fullness. Sometimes this can feel like chest pressure or nausea.
- Keep track of how much you are eating and drinking using a food log (journal, apps, etc.).
STAGE 3 SAMPLE MENU 1
8 AM 150-300 ml skimmed milk with 1 tablespoon oats.
- Instead of skimmed milk also prefer lactose-free milk .
10 AM 100-200 ml skimmed milk with 1 tablespoon of protein powder.
NOON 12 150-300 ml yogurt with 1 serving of fruit puree.
14 PM 100-200 ml apple puree.
18 PM 150-300 ml meat blender soup / 100 ml fruit puree.
20 PM 100-200 ml skimmed milk with 1 tablespoon of protein powder.
STAGE 3 SAMPLE MENU 2
8 AM Omelette ( 1 egg) (low fat)
10 AM 100 ml ayran / lactose free milk
NOON 12 Vegetarian puree and salmon puree (60 gr.)
14 PM Pineapple puree
18 PM Meat blender (60 gr.) + Vegetarian puree
20 PM 100-200 ml skimmed milk (lactose free)
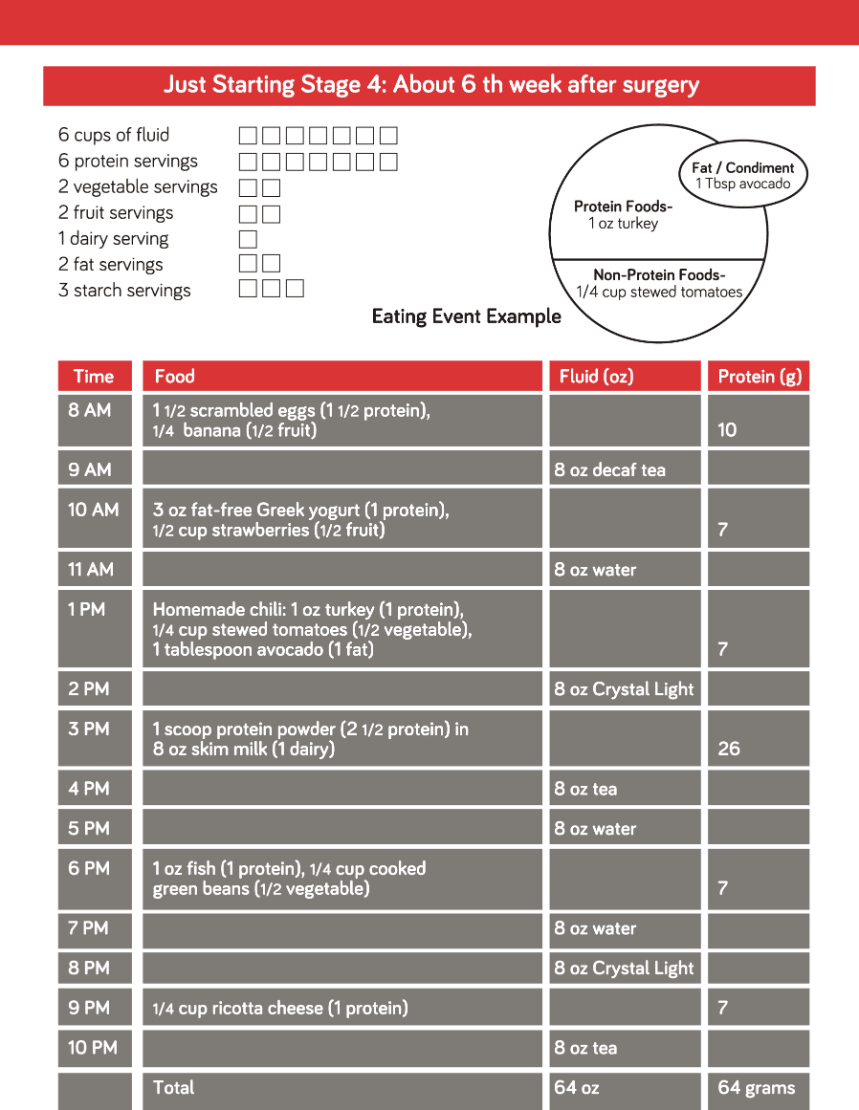
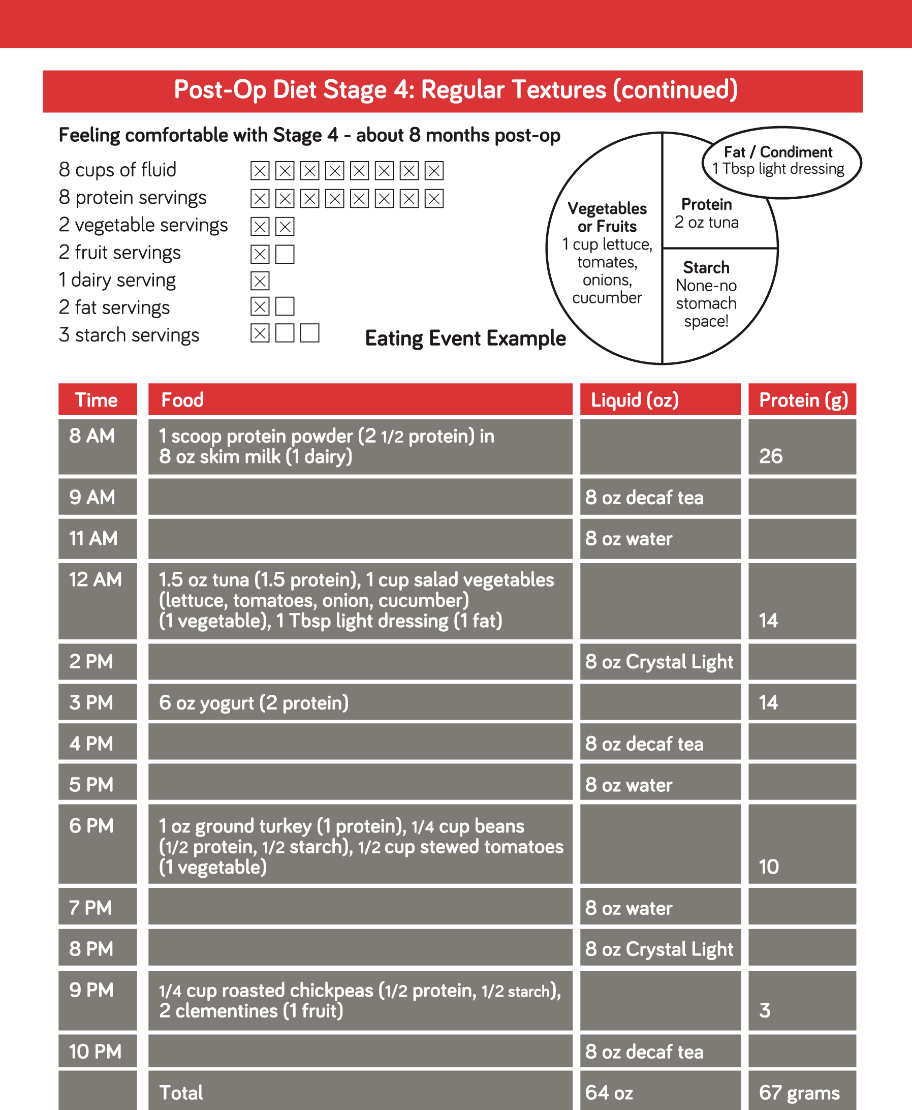
Post-Op Diet Stage 4: Regular Textures
Starts: 5 weeks after your surgery date
Last for: Lifelong, but your meal plan will change over time.
What to do: Keep sipping fluids. Use the meal plan below as guidance for a balanced diet. Keep taking vitamin and mineral supplements.
Fluid Goal: 48-64 ounces (1300-1700 ml) (fluid guidelines listed in stage 1)
Protein Goal: 60-70 grams/day
Meal Plan
8 cups of fluid _ _ _ _ _ _ _ _
8 protein servings _ _ _ _ _ _ _ _
2 vegetable servings _ _
2 fruit servings _ _
1 dairy serving _
3 starch servings _ _ _
How do I start in Stage 4?
- In Stage 4, you will start trying new types of foods. You may experience food intolerance, so be patient with your stomach. Tolerance improves with time. See below for possible ‘problem foods.’
- Use the meal plan for guidance. Each checkbox is a serving of food from that food group. In the early months after surgery, you won’t have room for all of the foods in the meal plan. Focus on foods from the protein, vegetable, and fruit groups first.
- The meal plan is not one size fits all. Your dietitian will help you change your meal plan as needed.
Possible ‘Problem Foods’
Your stomach can be sensitive for 3-6 months after surgery, and sometimes longer.
The following foods have unique textures that may be difficult to tolerate if eaten too soon.
Be cautious!
Protein: Tough red meat, hamburger, lobster, scallops, clams, shrimp
Fruits: Stringy, thick skins, peels (like oranges, grapes, pineapple)
Vegetables: Stringy, fibrous (like asparagus, peapods, celery)
Starches: Rice, pasta, doughy breads, popcorn
Sample Meal Plans
Eat protein foods first, then vegetables or fruits and eat starches last.
Use fats as a flavoring or to keep foods moist.
- This will be lifelong!
- Use your “Stage 4 Meal Ideas” handout for recipe ideas.
Self-monitor
- Track protein and fluids.
- Tracking regularly will help you stay accountable and more consistent with meeting your goals.
Listen to your stomach
- Stop eating at the first sign of fullness, which may feel like pressure in your upper chest.
Hunger may increase
- This is normal. The hormone changes from surgery might not last forever.
- Foods high in protein and fiber help control hunger, so fill up on these foods.
- Avoid eating out of habit or from behavioral triggers like boredom, stress and emotions.
Be aware of picking or grazing
- Are you eating something just because it’s available to you?
- Avoid unplanned eating moments and try to control your environment to minimize these opportunities.
- Have scheduled and structured eating times.
Work towards a balanced diet
- Learn which food groups the foods you eat belong to: Protein, Vegetable, Starch, etc.
- Work towards keeping these foods within the meal plan outlined by your dietitian.
These are examples to show you how the amount you can eat will change over time. Each person can choose their own foods based on their preferences and their tolerance.
Possible Problems and Solutions
We don’t expect all of these problems to happen to you, but if they do, we want you to know how to solve them. It is helpful to keep a record of anything unusual that occurs and what you did before and after it happened.
Dizziness, Headaches, Lightheadedness, Dark Urine (Signs of Dehydration)
Drink fluids with electrolytes (like Propel Zero, G2, Powerade Zero).
- Add salt to your foods.
- Drink salty bouillon or soup broth.
- Call the Physician’s Assistant phone line if you are unable to catch up on your fluids.
Constipation
Short-term Solutions
- Increase your fluids – aim for 64 ounces daily.
- Try a laxative, such as Milk of Magnesia or Miralax, and take a stool softener up to 3 times daily. • Try psyllium, a natural soluble fiber.
Long-term Solutions
- Increase your fluids – aim for 64 ounces daily (1800 ml).
- Increase your fiber intake. Eat more fruits, vegetables, and whole grains if your diet stage permits. If you are unable to add more fiber through your diet, try a fiber supplement, such as Benefiber or Metamucil.
- Slow and steady is the key to adding fiber to your diet. Start with a small amount, such as one serving of fiber supplement or one extra serving of food with fiber. Stick with that amount for 1-2 weeks before increasing as needed.
- Stay physically active.
- Continue taking a stool softener, if needed.
Diarrhea
- Limit or avoid foods with lactose. Lactose intolerance can occur after surgery. Please see page 9 for more details.
- Eat slowly and chew thoroughly.
- Do not drink fluids with meals.
- Avoid high sugar, high fat, and spicy foods.
- Limit the amount of sugar-free products (like sugar-free candies). These products may contain sugar alcohols (artificial sweeteners that end with –ol such as malitol, sorbitol, xylitol, etc.) that can cause diarrhea.
- Limit caffeinated beverages.
- Try a probiotic supplement – ask your dietitian for suggestions.
- Try psyllium, a natural soluble fiber.
Possible Problems and Solutions (continued)
Nausea and/or Vomiting
- Tune into your eating behaviors. Take small bites, chew thoroughly and pause after each bite.
- Stop eating or drinking at the first sign of fullness, which may feel like pressure in your upper chest.
- Stay hydrated. Drink at least 48-64 ounces of fluids.
- Keep foods tender and moist.
- Determine whether you might have lactose intolerance (page 9).
- Avoid eating and drinking at the same time.
- If these suggestions do not work, or you vomit bright red or dark brown liquid, please call the your surgeon’s office.
Bloating/Gas/Cramping
- Limit or avoid foods with lactose. Lactose intolerance can occur after surgery. Please see page 9 for more details.
- Limit or avoid sugar alcohols (artificial sweeteners that end with –ol such as malitol, sorbitol, xylitol, etc.).
- Avoid carbonated beverages.
- Don’t drink through a straw !!
Heartburn
- Every person has different food and beverage triggers for heartburn. Make a list of the ones that trigger heartburn for you and avoid them.
- Take your prescribed heartburn medication.
- Tune into your eating behaviors. Take small bites, chew thoroughly and pause after each bite. • Avoid lying down for 3-4 hours after eating.
Hair Loss
- Hair loss is normal in the first six months after surgery and will usually resolve on its own. If hair loss continues past six months, it may be related to nutrition.
- Meet your protein goal of 60-70 grams daily.
- Take your multivitamins daily – you should be getting 200% of iron, zinc, and biotin.
- You can also try Nioxin shampoo.
Vitamin and Mineral Supplements:
If you had a sleeve gastrectomy, you need the supplements at least 3 months. If you had a bypass, you will need to take vitamin and mineral supplements for the rest of your life after surgery. We recommend that you start with chewable or liquid supplements until stage 4. Over time, if you are comfortable swallowing a ‘petite’ tablet or cutting a pill in half, you can swallow your supplements.
Multivitamin with Minerals:
- Take a ‘complete’ multivitamin(s) daily; the dose will vary, based on the multivitamin brand.
- Complete multivitamins contain iron, zinc, folic acid, and copper.
Vitamin B12:
- Take 350-500 micrograms vitamin B12 daily in the form of a tablet or liquid.
- You can take vitamin B12 at any time or with any other supplements.
- You can also get vitamin B12 in a nasal spray or injection.
- Your multivitamin might have enough vitamin B12 in it.
Other Supplements:
Some patients may need extra vitamins and minerals, such as iron, vitamin D, or B vitamins. We will check your vitamin and mineral levels regularly through lab tests and discuss extra supplements as needed.
We wish you a happy and healthy life!





